FOLLICULAR STUDY
THE SERIAL MONITORING OF OVARIAN FOLLILCES AND ENDOMETRIUM
ALL YOUR QUESTIONS ANSWERED
Below is a Comprehensive Guide to Follicular Study for Successful Conception
A follicular study is one of the most effective ways to monitor ovulation and improve fertility outcomes. If you’re trying to conceive, this test helps determine the best time for conception and provides valuable insights into your reproductive health. In this guide, we’ll answer common patient questions & doubts about the follicular study, covering everything from the procedure to its importance in fertility treatments.
- What is a Follicular Study?
A follicular study is a series of ultrasound scans performed during the menstrual cycle to track the growth and rupture of ovarian follicles. Since follicles contain the eggs, monitoring their development helps determine the most fertile days for conception. Also the Endometrial thickness, that is the thickness of the lining of the endometrium is serially monitored.
- Why is a Follicular Study Important?
A follicular study helps:
✔ Identify the best time for natural conception
✔ Monitor the effects of fertility medications
✔ Diagnose ovulatory disorders
✔ Plan procedures like IUI (Intrauterine Insemination) and IVF (In-Vitro Fertilization)
✔ Detect issues like follicular rupture failure or poor egg development
If you’ve been struggling to conceive, your doctor may recommend a follicular study to assess your fertility.
- How is a Follicular Study Performed?
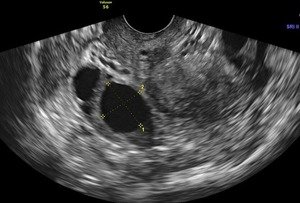
A follicular study is conducted through ultrasound scans, which can be either:
- Transvaginal ultrasound (TVS): A probe is inserted into the vagina for a clear view of the uterus and ovaries.
- Abdominal ultrasound: A probe is placed over the abdomen, usually requiring a full bladder for better visibility.
A transvaginal ultrasounds is usually preferred as it provide a detailed and accurate view of the endometrium follicles.
Transvaginal Ultrasonography is in fact the gold standard of assessment of the uterus & ovaries.
- When Should a Follicular Study Start?
The study typically begins on Day 8 to Day 10 of the menstrual cycle. The monitoring continues until ovulation occurs, which is usually around Day 11-14 in a 28-day cycle. However, cycle lengths vary, and the study is customised accordingly.
Sometimes, however the study is started as early as the 3rd day of the cycle for a baseline status and serial monitoring thereafter especially if injections are used for the ovulation induction treatment.
- How Many Ultrasounds Are Needed?
Usually, 3–5 scans are performed throughout the cycle. These scans track follicle growth, measure the endometrial thickness, and confirm whether ovulation has occurred. Sometimes if ovulation is delayed, the number of scans needed may be more.
- What is the Ideal Follicle Size for Ovulation?
The dominant follicle should ideally grow to 18–24 mm before ovulation. If the follicle reaches this size but doesn’t rupture, additional treatment may be needed.
- Is a Follicular Study painful?
No, the procedure is painless. A transvaginal ultrasound may cause mild discomfort, but it is generally quite well-tolerated.
- Do I Need Any Special Preparation for the Follicular Study?
- If an abdominal ultrasound is done, you may need a full bladder for a clearer image.
- For a transvaginal ultrasound, it’s best to have an empty bladder.
- Can I Try for Pregnancy During the Follicular Study?
Yes! Your doctor will guide you on the best days to try for natural conception based on the ultrasound results. If ovulation is detected, you will be advised to have intercourse during the most fertile window.
- Can a Follicular Study Detect Male Fertility Issues?
No, a follicular study only evaluates the female reproductive system. To assess male fertility, a semen analysis is required.
- What If No Dominant Follicle is Seen?
If no dominant follicle develops, it could indicate:
- Hormonal imbalances
- Polycystic Ovary Syndrome (PCOS)
Your doctor may suggest lifestyle changes, medications, or hormonal therapy to stimulate follicular development.
The important aspect is identifying the underlying problem so that it can be appropriately treated.
- What If Ovulation doesn’t occur Even with Follicle Growth?
Sometimes, follicles grow but fail to rupture, leading to a condition called Luteinized Unruptured Follicle Syndrome (LUFS). In such cases, doctors may prescribe injections for ovulation to occur or explore alternative fertility treatments it is persistent.
- How Does an Irregular Cycle Affect the Follicular Study?
Women with irregular cycles may require more frequent or prolonged monitoring to detect ovulation. If cycles are too unpredictable, doctors may recommend hormonal tests or ovulation induction medications.
- What Happens If My Follicular Study Shows an Issue?
If your follicular study indicates persistent poor follicular growth, lack of ovulation, or thin endometrial lining in repeated cycles your doctor may suggest:
✔ Ovulation induction medications (e.g., Clomiphene, Letrozole)
✔ Hormone therapy (for imbalances)
✔ Lifestyle changes to improve ovulation naturally
✔ Advanced fertility treatments like IUI or IVF
- Below are the normal serial changes in the uterine endometrium and ovarian follicles in the menstrual cycle. This will enable you to understand the basis and need for follicular study better.
A serial increase in endometrial thickness throughout the menstrual cycle typically follows these phases:
- Menstrual Phase (Days 1-5) → Thin, ~2-4 mm (Shedding of the old endometrial lining)
- Proliferative Phase (Days 6-14) → Gradually thickens to ~5-11 mm (Estrogen-driven growth)
- Ovulatory Phase (~Day 14) → ~8-12 mm (Triple-layer pattern, optimal for implantation)
- Secretory Phase (Days 15-28) → Thickest, ~10-16 mm (Progesterone stabilizes the lining for potential implantation)
- Follicular Growth Stages in the Menstrual Cycle
- Early Follicular Phase (Days 1-5)
- Multiple small follicles (2-5 mm) start developing under the influence of Follicle-Stimulating Hormone (FSH).
- No dominant follicle is selected yet.
- Mid-Follicular Phase (Days 6-10)
- One dominant follicle emerges and grows to 10-12 mm, while others regress.
- The follicle continues to grow at a rate of 1-2 mm per day.
- Late Follicular Phase (Days 11-14, Just Before Ovulation)
- The dominant follicle reaches 18-24 mm, indicating maturity.
- The follicle develops a fluid-filled antrum and prepares for ovulation.
- Ovulation (~Day 14 in a 28-Day Cycle)
- The follicle ruptures, releasing a mature egg.
- The size at rupture is typically 18-24 mm.
- The remaining follicle transforms into the corpus luteum, which secretes progesterone.
If medication in the form of injections and tablets are given for ovulation induction, there may be more than one or inface few to several dominant follicles.


Final Thoughts: Is a Follicular Study Right for You? A follicular study is a valuable tool for women trying to conceive naturally or undergoing fertility treatments. It helps pinpoint the best time for pregnancy and detects potential issues early especially if you’re struggling to conceive. The important aspect is identifying the underlying problem so that it can be appropriately treated.
